Is pelvic organ prolapse correction with vaginal mesh suitable with a correct indication and protocolized follow-up?
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Accepted: 25 January 2022
Authors
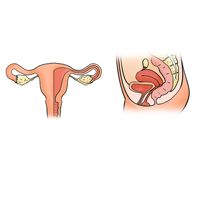
The use of vaginal mesh in order to correct Pelvic Organ Prolapse (POP) has been banned by the FDA due to the complications associated with them. The objective is to determine efficacy and safety in the short and long term in a sample of women undergoing transvaginal mesh surgery performed by properly trained surgeons, in a referral center and with a protocolized follow-up. We present a longitudinal, descriptive study of a cohort of 53 patients with POP who underwent transvaginal mesh surgery between 2001 and 2015. The efficacy of the treatment is evaluated quantifying both clinical changes and life quality, as well as the rate for prolapse recurrence and the short-and long-term treatment-related complications. A total of 53 patients with average follow-up of 87 months were included. All of them had their surgery performed by three properly-trained surgeons. Indication for mesh placement was assessed in 49.1% of cases due to previous surgery recurrence. Treatment improved urinary incontinence rates, constipation, voiding difficulty, dyspareunia and quality of life. Long-term complication rate was 9.6% (5.7% exposure, 1.9% urinary obstruction and 1.9% pain). None of the patients presented recurrence in the mesh-treated compartment and 6 patients (11.3%) needed surgery after recurrence in a different compartment at the end of follow-up. Vaginal placement of synthetic mesh for POP treatment is safe in the short-, medium- and long-term when performed in referral centers. The correct indication and long-term follow-up are essential to diagnose and treat possible complications.






