Complex vesicovaginal fistula: Analysis of patient characteristics and functional outcome of surgical reconstruction
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
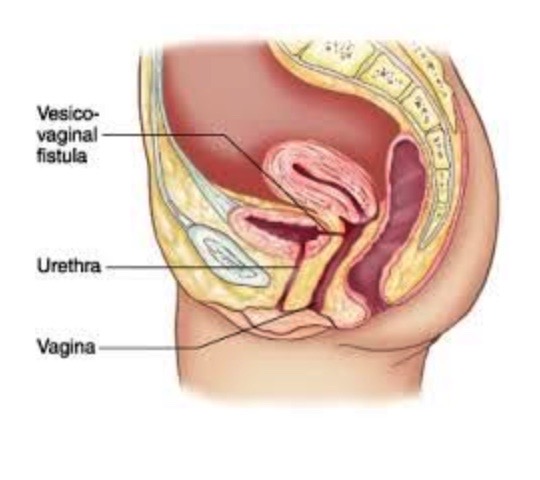
Complex vesicovaginal fistulas present a unique challenge to surgeons, and surgical reconstruction outcomes may be suboptimal. The aim is to evaluate the patient’s characteristics as well as the factors influencing the functional outcome of complex vesicovaginal fistula surgical reconstruction. From 2016 to 2020, the medical records of 28 patients with complex fistulas were analyzed retrospectively. Means, ranges, and standard deviations were used in descriptive analysis. For categorical data, the Fisher exact probability test was used. The mean (standard deviation) age at presentation was 44.4 (10.04) years, while 85.7% (24) of patients were below 50 years of age. Hysterectomy was the most common aetiology in 21 (75%) patients, followed by radiotherapy in 3 (10.7%). Surgical repair success was seen in 24 (85.7%) patients. Four (14.2%) patients had an unsuccessful repair, one vaginal and three abdominal approach. All the failed abdominal repairs were radiation-induced fistula (p=0.001). Other factors that significantly influenced repair failure include vaginal mucosal atrophy (3 failures out of 8 patients, p=0.013), severe fibrosis around the fistula (4 failures out of 12 patients, p=0.024), non-placement of suprapubic catheter (2 failures out of 3 patients, p=0.006), and non-placement of interposition tissue flap (p=0.005). Hysterectomy and radiotherapy are the common causes of complex vesicovaginal fistula. The outcome of the repair is hampered by vaginal mucosal atrophy and severe scarring. The use of a suprapubic catheter and an interposition tissue flap improves the outcome. Post-irradiation fistula has a significant impact on repair outcome and necessitates special consideration for a comprehensive management strategy.
How to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.






