Urinary symptoms and urodynamic findings before and after vaginal surgery for pelvic organ prolapse
Accepted: 15 June 2021
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
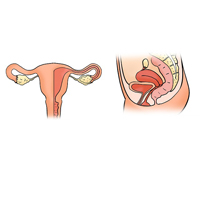
To ascertain the difference in urodynamic findings, specifically bladder sensation, and urinary symptoms after vaginal surgery for Pelvic Organ Prolapse (POP). Retrospective data analysis of 126 women who underwent vaginal surgery for POP without simultaneous anti-incontinence procedure from January 2013 to April 2019 at Siriraj Hospital, Thailand. Baseline characteristics, intraoperative details and pre and post-operative urinary symptoms and urodynamic findings were recorded. There was no significant difference in the pre and post-operative first desire to void, at 158±53 mL and 162±64 mL, respectively (p=0.518). Incidence of increased bladder sensation was also unchanged, from 46.0% to 46.8% (p=1.00). Post-operative urodynamic stress incontinence was significantly increased, from 15.9% to 31.0% (p=0.003), as was the incidence of weak bladder contractility index (<100), from 47.3% to 61.8% (p=0.005). Significant improvements in post-operative urge urinary incontinence, urgency and voiding dysfunction were noted, from 50.8% to 31.7% (p=0.001), 63.5% to 38.9% (p<0.001) and 42.9% to 5.6% (p<0.001), respectively. No significant difference in bladder sensation after vaginal surgery for POP repair was noted. However, urinary symptoms significantly improved after surgery.
How to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.
An Open Access Publication is one that meets the following two conditions:
- the author(s) and copyright holder(s) grant(s) to all users a free, irrevocable, worldwide, perpetual right of access to, and a license to copy, use, distribute, transmit and display the work publicly and to make and distribute derivative works, in any digital medium for any responsible purpose, subject to proper attribution of authorship, as well as the right to make small numbers of printed copies for their personal use.
- a complete version of the work and all supplemental materials, including a copy of the permission as stated above, in a suitable standard electronic format is deposited immediately upon initial publication in at least one online repository that is supported by an academic institution, scholarly society, government agency, or other well-established organization that seeks to enable open access, unrestricted distribution, interoperability, and long-term archiving.
Authors who publish with this journal agree to the following terms:
- Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal.
- Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgement of its initial publication in this journal.
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
Similar Articles
- Colin Walsh, Wendy Allen, Katrina Parkin, Chinmoy Mukerjee, Kate Moore, Low-count bacteriuria in refractory idiopathic detrusor overactivity versus controls , Urogynaecologia: Vol. 25 No. 1 (2011)
You may also start an advanced similarity search for this article.

 https://doi.org/10.4081/uij.2021.264
https://doi.org/10.4081/uij.2021.264



